

You got the scan. You did the thing.
Now you're staring at a multi-page report filled with percentages, regional breakdowns, and terms like "visceral adipose tissue" that seem designed to confuse rather than clarify.
Many people leave their DEXA appointment with precise data and zero idea what to do with it.
That's a problem. Because a DEXA scan delivers the most accurate snapshot of body composition available outside a research laboratory.
It measures exactly where fat and muscle sit in your body, how your bone density compares to healthy baselines, and whether hidden metabolic risks exist beneath the surface.
The numbers matter. But they only become valuable when you understand what they reveal about your health trajectory.
Let’s break down every section of a DEXA report so you can transform raw data into actionable decisions. Here's what you need to know.
DEXA stands for Dual-Energy X-ray Absorptiometry. The technology uses two low-energy X-ray beams at different intensities to differentiate between bone mineral content, lean tissue, and fat mass throughout your entire body.
Originally developed to measure bone density for osteoporosis screening, DEXA has become the gold standard for precise body composition analysis.
The scan itself takes approximately 10 to 15 minutes.
You lie on a padded table while a mechanical arm passes over your body, capturing detailed images that software translates into comprehensive metrics. Radiation exposure is minimal, roughly one-tenth of a standard chest X-ray, according to RadiologyInfo.
What makes DEXA superior to alternatives like bioelectrical impedance scales or skinfold calipers?
Its ability to measure fat you cannot see or feel. The scan detects fat stored around internal organs, imbalances between left and right sides of your body, and changes in specific regions over time. This precision transforms body composition from a vague concept into measurable, trackable data.
DEXA scanning operates with a margin of error between 1% and 2% for body fat measurements.
Compare this to the alternatives:
BMI fails to distinguish between muscle and fat entirely. Bioelectrical impedance devices carry error margins of 5% to 15%. Even hydrostatic weighing cannot pinpoint regional fat distribution.
This precision becomes particularly valuable when tracking progress over time. A 2% shift in body fat percentage represents a significant physiological change, and DEXA can reliably detect these shifts. Other methods would chalk them up to measurement noise.
One important caveat:
DEXA measures all fat in your body, including essential fat in the brain, bone marrow, and organs. This is why DEXA-reported body fat percentages often run slightly higher than numbers from other testing methods. The reading isn't inflated. It's simply more comprehensive.
Total body fat percentage represents the proportion of your mass composed of adipose tissue.
The number itself means little without context. Your age, biological sex, activity level, and personal health goals all influence what constitutes an optimal range for you specifically.
General reference ranges based on American Council on Exercise guidelines provide useful starting benchmarks:
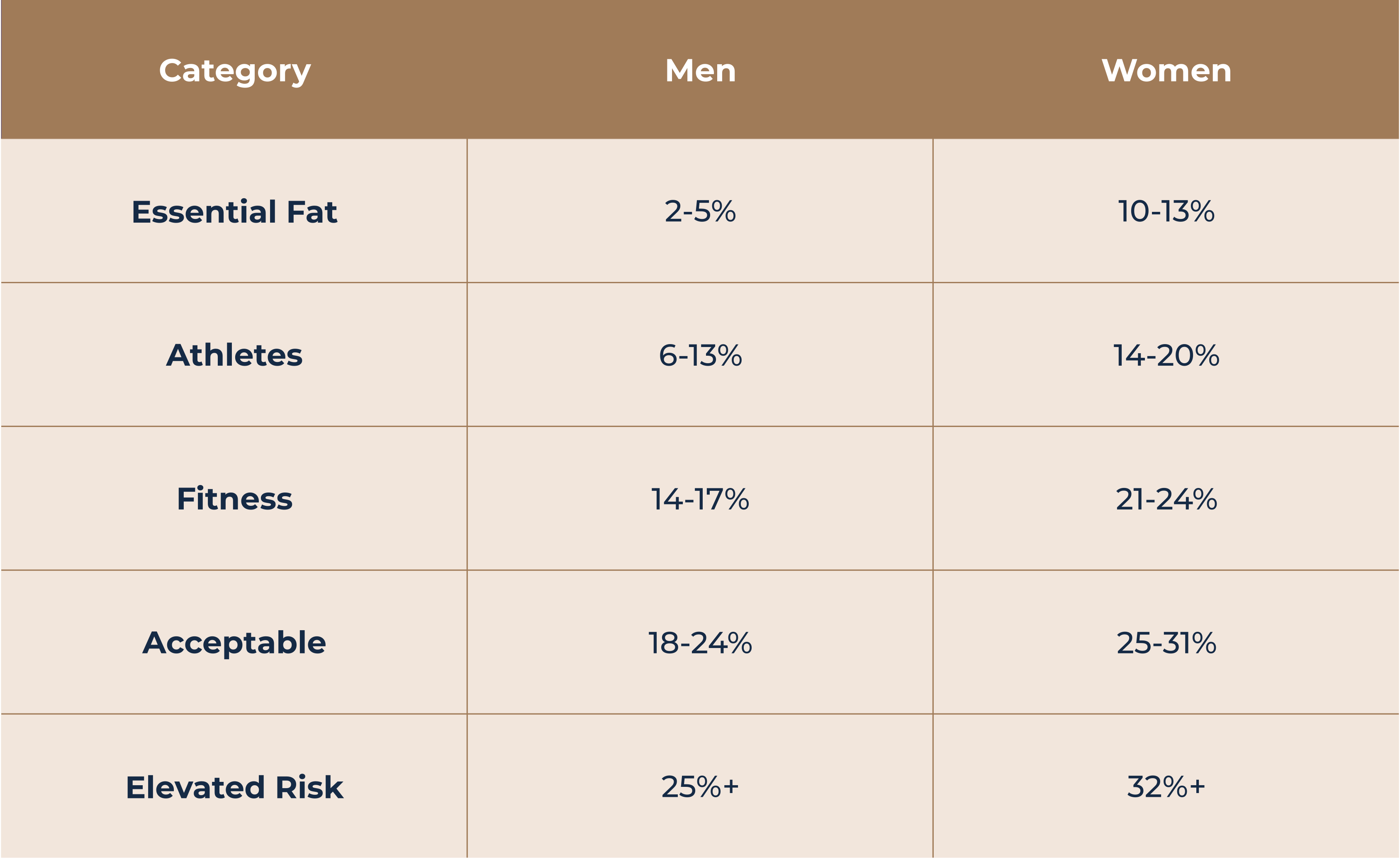
These ranges represent population averages, not prescriptive targets. A 45-year-old executive focused on longevity has different optimal body composition than a competitive endurance athlete. A DEXA report provides the raw measurement. Interpreting what that number means for your specific situation requires clinical context.
Context determines the answer.
For men, 20% body fat falls within the acceptable healthy range but sits above the fitness category. For women, 20% represents athletic-level leanness that may be difficult to maintain without dedicated training.
The more relevant question isn't whether a single percentage hits an arbitrary threshold. What matters is how that number relates to your metabolic health markers, visceral fat levels, and personal performance goals.
A man with 20% body fat and elevated visceral fat faces different health considerations than someone with the same percentage but fat distributed primarily subcutaneously.
Visceral adipose tissue (VAT on most reports) represents fat stored around internal organs within your abdominal cavity. This metabolically active fat behaves differently from the subcutaneous fat you can pinch beneath your skin.
And it's far more dangerous.
Research published in the journal Circulation established visceral fat as an independent predictor of cardiovascular disease, type 2 diabetes, and metabolic syndrome, even when total body fat remains within normal ranges.
High visceral fat triggers inflammatory responses, disrupts hormone signaling, and impairs insulin sensitivity in ways that subcutaneous fat does not.
Your DEXA report typically displays VAT in grams or as a risk category. Reference ranges vary by scanner manufacturer, but generally:
Here's the encouraging news:
Visceral fat responds more readily to lifestyle modifications than stubborn subcutaneous deposits.
Structured exercise programs combining resistance training with cardiovascular activity, along with dietary adjustments reducing processed foods and alcohol, can produce measurable VAT reductions within 8 to 12 weeks.
DEXA reports break down fat storage into two key regions: android (abdominal) and gynoid (hip and thigh). The ratio between these regions reveals metabolic risk patterns that total body fat percentage alone cannot capture.
Android fat distribution creates the classic "apple" body shape, with fat concentrated around the midsection. Gynoid distribution produces a "pear" shape, with fat stored primarily in the lower body.
Research consistently links android-dominant patterns to higher cardiovascular and metabolic risk, regardless of total fat mass.
The A/G ratio on your report divides android fat percentage by gynoid percentage. Optimal ranges differ by sex:
A ratio exceeding these thresholds doesn't guarantee health problems. But it does indicate where attention might yield the greatest risk reduction. If your A/G ratio is elevated, you'll benefit more from interventions targeting abdominal fat than from generalized weight loss efforts.
Beyond fat measurement, DEXA quantifies lean tissue mass, encompassing muscle, organs, connective tissue, and water.
For those focused on fitness performance and longevity, tracking lean mass over time reveals whether your training and nutrition protocols are actually producing the adaptations you're working toward.
DEXA reports display lean mass totals broken down by region: arms, legs, and trunk. This segmentation serves two important purposes:
Some DEXA reports include an RSMI calculation using the Baumgartner equation. This metric compares appendicular lean mass (the sum of lean mass in your arms and legs) to height, providing a standardized assessment of muscle mass relative to body size.
Clinical thresholds for sarcopenia, the age-related loss of muscle mass and function, sit at:
Values approaching these thresholds in middle age signal an opportunity for early intervention through progressive resistance training and adequate protein intake. The time to address muscle loss is before it becomes a problem.
While body composition analysis may have motivated your DEXA scan, the bone density data included in the report deserves attention, particularly if you're over 40 or have a family history of osteoporosis.
Your T-score compares bone mineral density to that of a healthy 30-year-old of the same sex, representing peak bone mass. The World Health Organization defines categories as follows:
Your Z-score compares density to age-matched peers, revealing whether your bones are stronger or weaker than expected for someone of similar age. A Z-score below -2.0 may indicate secondary causes of bone loss worth investigating with your physician.
Bone density responds to weight-bearing exercise, adequate calcium and vitamin D intake, and certain medications when indicated. Early detection of declining bone mass creates opportunity for intervention before fracture risk becomes significant.
Proper preparation maximizes the accuracy and comparability of your results across multiple scans.
24 hours before your appointment:
Day of your scan:
For consistent tracking across scans:
The scan itself requires no special preparation beyond these considerations. You lie still on the table for approximately 10 to 15 minutes while the scanner completes its passes.
Raw data becomes valuable only through interpretation and action. This framework helps transform a DEXA report into a roadmap for improvement.
For a first scan, the results establish the baseline against which all future progress will be measured. Record your total body fat percentage, visceral fat mass, lean mass by region, and bone density scores. These numbers represent a starting point, not a verdict on your overall health.
Your results may reveal multiple areas for potential improvement. Rather than attempting to address everything simultaneously, identify the metric presenting the greatest health risk or the most meaningful opportunity.
If you have elevated visceral fat and borderline bone density, you might prioritize visceral fat reduction initially. The lifestyle modifications involved, like increased exercise and improved nutrition, often benefit bone health concurrently.
Vague intentions like "lose weight" or "get healthier" lack the specificity needed for accountability.
DEXA data enables precise goal-setting: reduce visceral fat by 30 grams over 12 weeks, maintain lean mass within 2% while reducing total body fat by 3 percentage points, or improve T-score by 0.3 over 18 months.
DEXA scans generate medical-grade data that benefits from professional interpretation. Reports may reveal patterns you cannot identify without clinical training. A physician experienced in longevity medicine and preventive care can contextualize results within your complete health picture, including blood markers, genetic factors, and personal history.
Single measurements provide snapshots. Trends reveal the true story.
Most people benefit from repeat scans every 3 to 6 months when actively pursuing body composition changes, or annually for maintenance monitoring. Consistent intervals between scans allow meaningful comparison of progress.
Yes. For anyone serious about optimizing health rather than chasing scale weight, DEXA scanning provides unmatched value. The technology reveals what no mirror, scale, or BMI calculator can show: the composition and distribution of tissue within your body.
The investment proves particularly worthwhile if you:
Scan costs typically range from $150 to $300 depending on location and provider, which is a small fraction of what many people spend annually on supplements or fitness equipment that may or may not be producing results.
What matters more than the scan itself is what happens with the information. Data without action changes nothing. Data paired with expert interpretation and a personalized implementation plan becomes a powerful tool for extending your healthspan.
DEXA scan results provide precise insights into your current body composition, surpassing the accuracy of guesswork and bathroom scales. But numbers on a report represent potential, not progress. The value emerges when those metrics inform a structured, personalized approach to health management.
At PrimaryMD, DEXA scanning forms one component of a comprehensive diagnostic protocol. Members receive expert interpretation of their results alongside a 100-biomarker blood panel, VO₂ max testing, and genetic analysis, all synthesized into an actionable health plan tailored to your specific physiology and goals.
Rather than handing you data and sending you on your way, your PrimaryMD physician and wellness expert work alongside you to translate insights into sustained improvements. Your care team monitors your wearable data, asks questions, adjusts your protocols, and checks in proactively, with monthly sessions from your wellness expert and quarterly visits with your physician.
Your health deserves more than a scan and a shrug. Join the waitlist and experience healthcare built around you.
If you're actively working to change your body composition, every 3 to 6 months provides enough time to see measurable changes while keeping you accountable. For maintenance monitoring, annual scans track long-term trends in bone density and lean mass preservation.
Insurance typically covers DEXA scans for bone density screening (especially for women over 65 or those with osteoporosis risk factors) but rarely covers body composition analysis. Most people pay out-of-pocket for comprehensive body composition DEXA scans, with costs ranging from $150 to $300.
Different scanner manufacturers and models may produce slightly different readings. For the most accurate tracking over time, use the same facility and scanner for all your scans. If you must switch, note the change and expect some variation unrelated to actual body composition changes.
Body fat scales use bioelectrical impedance, which estimates body fat based on how quickly an electrical current passes through your body. These scales carry error margins of 5% to 15% and cannot measure visceral fat or regional distribution. DEXA provides 1-2% accuracy and complete regional breakdown.
Wear comfortable, loose-fitting clothing without metal components. No zippers, underwire bras, or metal buttons. Athletic wear typically works well. You'll also need to remove jewelry and any metal accessories before the scan.