

You've optimized your calendar, your investments, your team.
But when was the last time you got precise data on what's happening inside your body?
Bone density loss and changes in body composition begin earlier than most men realize.
A DEXA scan (Dual-Energy X-ray Absorptiometry) provides the most accurate measurement of bone density and body composition available.
The technology has evolved beyond its original purpose of detecting osteoporosis. Modern DEXA scans now offer comprehensive insights into visceral fat levels, muscle mass distribution, and metabolic health markers that directly influence longevity and disease risk.
For men over 40 who prioritize long-term health and performance, understanding when to undergo a DEXA scan and how to interpret the results can transform how you approach exercise, nutrition, and medical care.
Your body starts shifting in your 40s.
Bone density declines about 0.5–1% per year starting around age 30–40 in men. Women experience a sharper, rapid decline during menopause, but men’s steady loss is often unnoticed until a fracture occurs.
Muscle loss (sarcopenia) begins early too. Adults lose 3–5% of muscle mass per decade after age 30, and by age 60, 5–13% meet criteria for sarcopenia depending on the diagnostic method used.
For anyone aiming to preserve strength, performance, and long-term mobility, getting a DEXA baseline in your 40s gives your physician the data needed to spot early changes and adjust training, nutrition, or treatment before problems surface.
Want that baseline before problems surface? PrimaryMD includes DEXA scanning in every membership.
Medical organizations provide these specific recommendations for bone density testing (DEXA) in men:
These focus on osteoporosis prevention. For optimizing body composition, visceral fat, or early muscle loss, clinicians often recommend baseline DEXA at age 40 with tailored follow-ups.
Certain factors elevate your risk for bone loss, unfavorable body composition changes, or metabolic dysfunction. The presence of any of these factors may justify earlier or more frequent DEXA scanning:
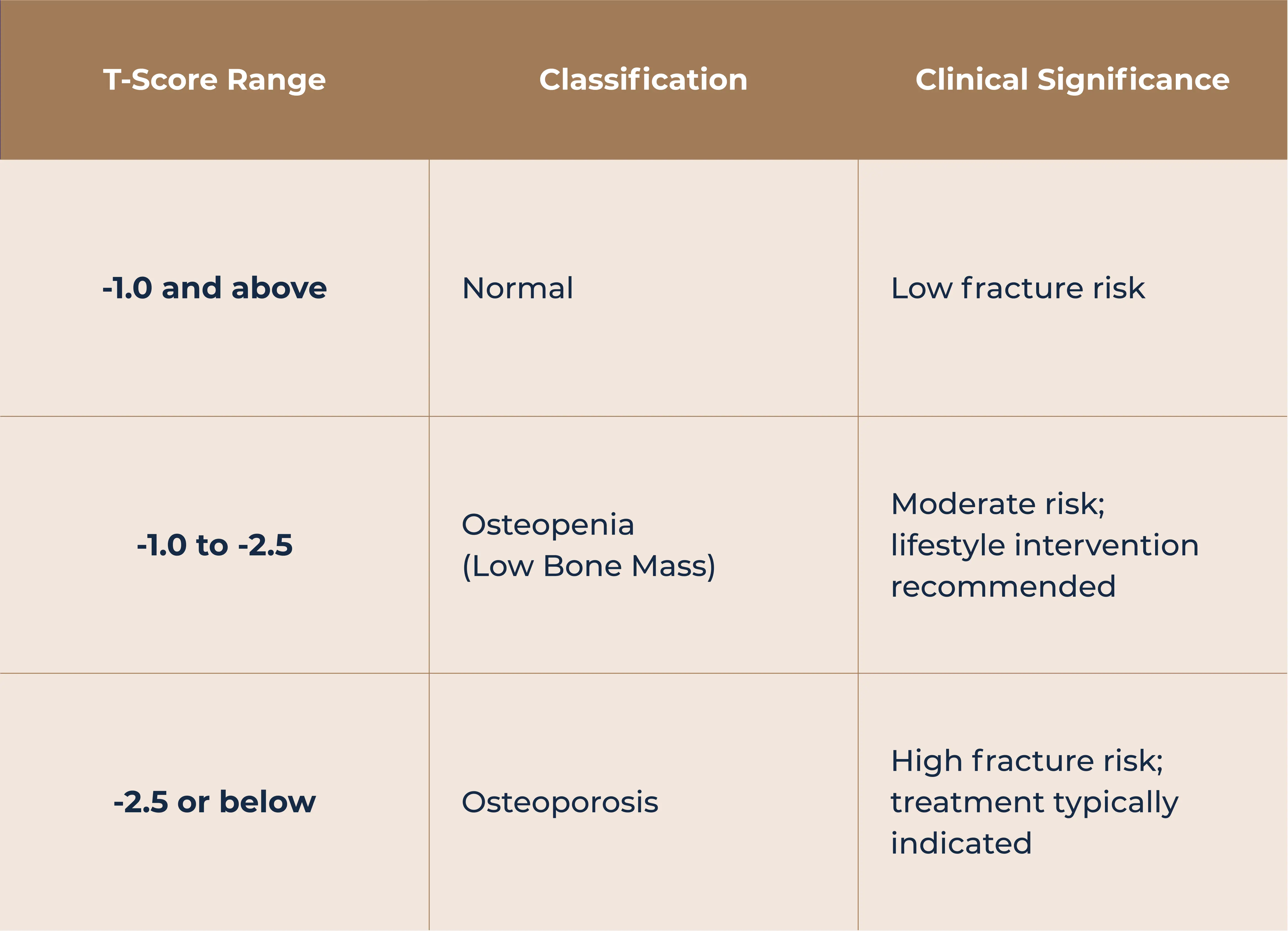
DEXA results for bone density are reported using standardized scores that compare your measurements to reference populations.
The T-score compares your bone density to the optimal peak density of a healthy 30-year-old of the same sex.
For men aged 50 and older, T-scores serve as the primary diagnostic criterion for bone health assessment.
The Z-score compares your bone density to others of the same age, sex, and ethnicity. This score is particularly useful for men under 50 or for identifying whether bone loss exceeds what would be expected for your age group.
A Z-score of -2.0 or lower is defined as below the expected range for age and may warrant investigation for underlying causes.
Modern DEXA technology provides extensive data on body composition that extends well beyond bone density measurements. These metrics provide actionable insights for men seeking to optimize their health and physical performance.
DEXA quantifies both total body fat percentage and its distribution across different regions. The android-to-gynoid ratio describes whether you carry fat predominantly around your midsection (apple shape) or around your hips and thighs (pear shape).
From a health risk perspective, values below 1.0 for men indicate a more favorable fat distribution pattern. Higher ratios suggest increased metabolic risk even when total body fat remains within acceptable ranges.
Visceral fat represents one of the most clinically significant measurements available from a DEXA scan. This metabolically active fat surrounds internal organs and produces inflammatory compounds that interfere with hormone function, appetite regulation, and insulin sensitivity.
Research published in the journal Obesity found that visceral fat is an independent predictor of all-cause mortality in men, regardless of total body weight.
Clinical thresholds typically classify visceral fat measurements as follows:
Data shows that visceral fat increases with age, and once you reach the 50th percentile for overall body fat, visceral fat levels may double between your 20s and 50s.
Appendicular lean mass (ALM) measures the muscle mass in your arms and legs. This metric serves as the primary indicator for sarcopenia diagnosis when adjusted for height or BMI.
Research cutoffs generally define low muscle mass as:
Tracking lean mass over time allows you to assess whether your training programs effectively preserve or build muscle. A decline in lean mass despite consistent exercise may indicate the need for nutritional adjustments, particularly increased protein intake, or signal underlying health issues requiring medical attention.
Sarcopenia, the age-related loss of skeletal muscle mass and function, has been recognized as an independent medical condition by the International Classification of Diseases. The condition affects both quality and quantity of life, increasing risks for falls, fractures, disability, and mortality. DEXA scanning serves as the gold standard for measuring muscle mass in sarcopenia diagnosis.
The European Working Group on Sarcopenia in Older People defines the condition using a combination of low muscle mass (measured by DEXA) plus either low grip strength or slow walking speed.
Early detection through regular DEXA monitoring allows for timely intervention with progressive resistance training and nutritional optimization before functional decline becomes apparent.
You might believe you're immune to sarcopenia if you prioritize strength training. However, subclinical muscle loss can occur even in active individuals, particularly those who emphasize cardiovascular exercise over resistance training.
Baseline DEXA measurements provide objective evidence of current muscle mass status and enable tracking of changes over subsequent years.
At PrimaryMD, these metrics integrate into comprehensive health assessments, connecting body composition data with personalized fitness and nutrition guidance from your dedicated care team.
Optimal DEXA scanning frequency depends on your baseline results, risk factors, and health objectives.

The Endocrine Society recommends BMD testing at the spine and hip every one to two years to assess treatment response in men receiving osteoporosis therapy. For those with stable bone density, the frequency of measurements may be reduced.
For body composition monitoring in healthy men without osteoporosis, many longevity-focused clinicians recommend scans every 6 to 12 months when actively working on fat loss or muscle gain.
This interval provides sufficient time for measurable changes while maintaining momentum toward goals. Once optimal body composition is achieved, annual scans typically suffice for ongoing surveillance.
Repeat DEXA scans should ideally be performed at the same testing center using the same equipment. This consistency improves the accuracy of comparisons between scans and reduces the risk of measurement variability affecting interpretation.
Proper preparation helps produce the most accurate DEXA results. Following these guidelines before your appointment maximizes the reliability of your measurements.
24 hours before:
Day of your scan:
During the scan, you lie still on the table while the scanner arm passes over your body. The technologist may position your legs on a padded box and adjust your foot placement to optimize hip imaging. The entire process typically concludes within 15 to 20 minutes.
Raw DEXA data requires clinical interpretation to become actionable health guidance. Working with a physician who understands both the technical aspects of DEXA analysis and the practical application of results to lifestyle medicine produces the best outcomes.
If your T-scores fall between -1.0 and -2.5 (osteopenia), prioritize weight-bearing exercise, adequate calcium intake of 1000 to 1200 mg daily, and vitamin D levels of at least 30 ng/mL.
The Endocrine Society recommends 30 to 40 minutes of weight-bearing activity three to four times per week. Smoking cessation and alcohol moderation become particularly important, as current smoking increases hip fracture risk by approximately 80% in men.
If your T-scores are -2.5 or below, or you have osteopenia plus elevated fracture risk calculated through tools like FRAX, you may benefit from pharmacological treatment. Options include bisphosphonates and other bone-active agents that have demonstrated fracture reduction in clinical trials.
Elevated visceral fat responds well to caloric restriction combined with resistance training.
Visceral fat is highly responsive to weight loss, and people often lose a disproportionately large amount of visceral fat during dieting compared to other fat stores.
Tracking progress through periodic DEXA scans validates whether interventions are producing the desired internal changes, even when scale weight remains stable.
For men working to preserve or build muscle mass, DEXA provides objective feedback on whether protein intake and training stimulus are sufficient. A decline in lean mass despite consistent effort may indicate the need for nutritional adjustments or investigation of underlying hormonal or metabolic factors.
At PrimaryMD, your physician and wellness expert work together to translate these metrics into sustainable lifestyle changes, adjusting your personalized care plan as your body composition evolves.
Men who take a proactive approach to health monitoring gain advantages that reactive medical care cannot provide. DEXA scanning offers objective measurements that remove guesswork from fitness programs, nutritional strategies, and medical decisions.
The best time to establish baseline measurements is before problems become apparent. A DEXA scan in your 40s creates reference points that make future changes unmistakably clear.
At PrimaryMD, DEXA scanning is one component of your comprehensive diagnostic protocol. Members also receive a 100-biomarker blood panel, VO2 max testing, genetic analysis, and ongoing wearable integration to monitor trends in real time.
Your dedicated care team, including your physician, wellness expert, and care coordinator, synthesizes this data into a personalized health strategy built around your goals.
Your health deserves more than annual physicals and reactive care. Join the PrimaryMD waitlist to experience healthcare designed around you.
Yes. DEXA uses very low radiation doses, typically in the single-digit microsievert range. This exposure is comparable to or less than a chest X-ray and far lower than CT scanning. The radiation is similar to what you would receive during a short domestic flight from natural background sources.
Clinical guidelines recommend routine bone density screening beginning at age 70, or earlier for men aged 50 to 69 with risk factors. For proactive body composition monitoring, many longevity physicians suggest establishing a baseline around age 40 to track changes over time.
Yes. Unlike waist circumference or BMI, DEXA directly measures visceral fat deposits around internal organs. A man with apparently normal external appearance can carry unhealthy amounts of visceral fat that only DEXA can quantify accurately.
DEXA provides superior accuracy compared to bioelectrical impedance scales, skinfold calipers, or hydrostatic weighing. While MRI offers similar precision, it costs significantly more and takes longer. DEXA represents the optimal balance of accuracy, convenience, and cost for regular body composition monitoring.
Costs typically range from $75 to $300 depending on location and provider. Insurance may cover bone density screening for men over 70 or those with documented risk factors, but body composition analysis is usually out-of-pocket. PrimaryMD members receive DEXA scans as part of their membership.