

Somewhere between 40 and 55, your body starts making decisions without you.
Bone density quietly declines. Visceral fat accumulates around organs you can't see. Muscle mass erodes so gradually you blame the mirror, not the loss.
None of it shows up on a scale. None of it announces itself until something breaks, tears, or stops working the way it should.
Here's what makes this particularly costly for high performers:
By the time you notice, you've already lost years of intervention time. The executive who discovers osteopenia at 48 has options. The one who discovers osteoporosis at 64 has damage control.
Standard screening guidelines tell you to wait until 65. Those guidelines were written for average risk in average populations. They weren't written for you.
A DEXA scan takes 15 minutes. It measures bone density at the spine and hip, plus body composition down to regional fat distribution and lean muscle mass. It tells you exactly where you stand, so you can decide exactly what to do about it.
Skip the 'should I' debate. Focus on how much runway you want between knowing and acting.
The Bone Health and Osteoporosis Foundation (BHOF) recommends routine bone-density screening for women at 65 and men at 70. And earlier testing for adults 50 and older who have risk factors such as prior fractures, long-term steroid use, or medical conditions that weaken bone.
For those who want a more proactive approach, establish a baseline in your 40s or early 50s to track long-term trends, even though this is earlier than formal guidelines.
Why this window? It captures your bone density and body composition before age-related decline accelerates significantly.
Women experience the most rapid bone loss during the four to five years surrounding menopause. Men experience more gradual decline, though factors common among executives (chronic stress, irregular sleep, sedentary periods, and certain medications) can accelerate this process.
You may benefit from getting your first DEXA scan sooner if you have:
Establishing a baseline earlier allows subsequent scans to measure your individual rate of change rather than comparing results only to population averages. That's the difference between knowing where you stand and knowing where you're headed.
A DEXA scan measures bone mineral density at the spine and hip using low-dose X-rays. The procedure takes approximately 15 minutes, requires no preparation, and involves no injections.
Total body DEXA scans also provide detailed analysis of body composition:
This level of precision lets you detect changes that would never register on a bathroom scale or in a standard physical exam.
For executives who invest in fitness programs, nutrition protocols, or wellness interventions, DEXA provides objective validation. Subsequent scans confirm whether your efforts are producing measurable improvements in lean mass, reductions in visceral fat, or maintenance of bone density.
You're not guessing. You're measuring.
Identifying osteopenia (low bone density) or elevated visceral fat in your forties provides significantly more intervention options than detection in your sixties.
You bear responsibility not only for your own well-being but often for organizations, teams, and stakeholders who depend on your continued leadership. From this perspective, proactive health management represents a form of risk mitigation.
The direct medical costs of a hip fracture average $40,000 to $60,000. But for executives, the indirect costs often exceed these figures substantially: extended recovery periods, reduced capacity during rehabilitation, and potential long-term limitations. A preventable fracture at age 62 can significantly alter your career trajectory and quality of life for decades.
Body composition changes affect more than physical health. Research associates elevated visceral adipose tissue with systemic inflammation, insulin resistance, and cognitive effects including reduced mental clarity and increased fatigue. Declining muscle mass is associated with reduced energy levels, poorer sleep quality, and decreased physical resilience.
These changes occur gradually. They're often attributed to "normal aging" rather than recognized as modifiable physiological factors.
Regular DEXA scanning objectively identifies these trends, allowing for targeted intervention before cumulative effects impact your daily function and professional performance.
Following an initial baseline scan, the frequency of subsequent testing depends on your results and individual risk factors.
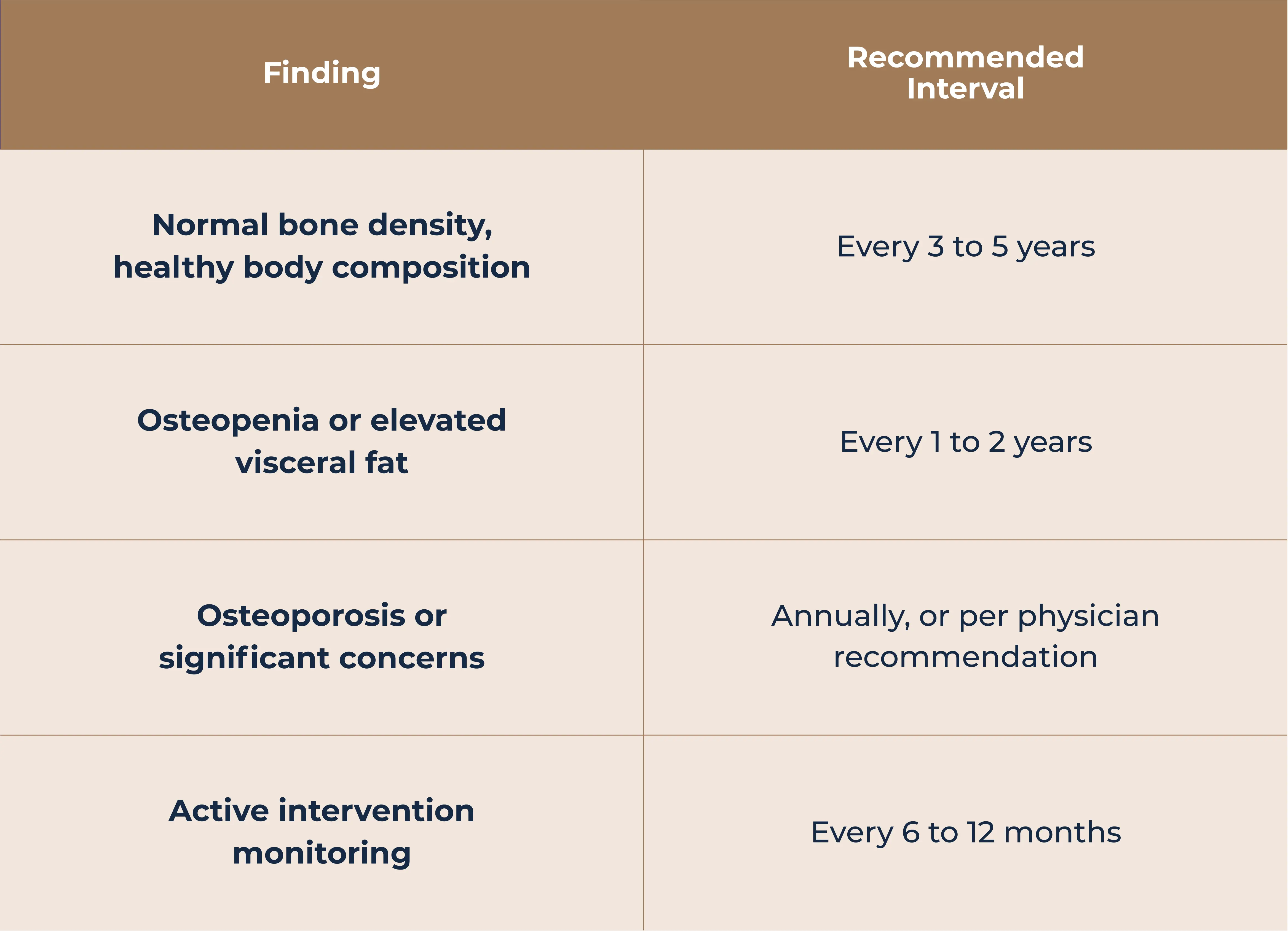
Executives actively pursuing body composition goals or tracking their response to lifestyle interventions often benefit from annual scans, regardless of baseline results. This frequency provides sufficient data points to evaluate trends and calibrate ongoing efforts.
DEXA results include T-scores (comparing bone density to healthy young adults) and Z-scores (comparing to age-matched peers).
Body composition results quantify total body fat percentage, regional fat distribution, visceral adipose tissue, and lean mass. These metrics offer a comprehensive view of metabolic health that extends beyond what weight or BMI can reveal.
Normal results: Continue current health practices. Use baseline data for future comparison. Schedule follow-up in 3 to 5 years.
Low bone density: Work with your physician to discuss intervention options. These may include resistance training, optimizing calcium and vitamin D levels, lifestyle modifications, or medication, depending on severity and risk factors.
Elevated visceral fat: Address through targeted nutrition, consistent exercise combining cardiovascular and resistance training, sleep optimization, and stress management. Follow-up scanning can confirm improvement.
Declining lean mass: Evaluate resistance training protocols and protein intake. Early sarcopenia responds well to intervention at any age.
The value of DEXA data lies in translating findings into specific, monitored action plans.
DEXA scanning is most valuable as one component of a thorough health evaluation. Combined with advanced bloodwork, cardiovascular fitness testing, and detailed health history review, DEXA results contribute to a complete picture of your current health status and trajectory.
At PrimaryMD, DEXA scans are included in your comprehensive diagnostic assessment alongside 93+ marker blood panels, VO2 max testing, RMR assessments, and wearable integration. Your care team uses this data to build a personalized care plan that addresses the full scope of your health goals.
The process starts with automated collection of your complete medical history from previous providers. Then you undergo baseline testing that far exceeds standard physical exams. Your 2-hour intake session with your physician focuses on understanding your story and creating a care plan built around your specific goals.
For executives accustomed to data-driven decision making in their professional lives, this approach brings the same rigor to personal health management.
Traditional healthcare models focus on addressing problems after they develop. For many conditions, including osteoporosis and metabolic dysfunction, this means intervention begins only after significant progression has occurred.
Proactive screening shifts this timeline forward. A 15-minute DEXA scan provides information that can guide prevention for decades.
For executives who recognize health as foundational to sustained professional performance, establishing baseline measurements and monitoring changes over time represents a sound investment in long-term capability.
Your health data should be as precise as your business metrics.
At PrimaryMD, DEXA scans are part of a comprehensive diagnostic assessment that includes advanced blood panels, VO2 max testing, body composition analysis, and continuous wearable monitoring. Your dedicated care team, including your physician, wellness expert, and care coordinator, uses this data to build a personalized plan designed around your goals.
You get 24/7 access to your care team, quarterly physician visits, monthly wellness sessions, and the advanced diagnostics that proactive health management requires.
Join the PrimaryMD waitlist to experience healthcare built around you.
For proactive health optimization, consider establishing your baseline between ages 40 and 50. This captures your bone density and body composition before age-related decline accelerates, giving you data to track your individual trajectory over time.
For normal results, every 3 to 5 years is typically sufficient. If you have osteopenia, elevated visceral fat, or are actively monitoring body composition goals, annual scans provide better trend data. Those with osteoporosis or on treatment should follow their physician's recommendations, which may be every 6 to 12 months.
DEXA provides precision measurements of bone mineral density, total body fat percentage (accurate within 1-2%), lean muscle mass, and visceral adipose tissue. Standard bloodwork, clinical exams, and bathroom scales cannot measure these metrics with comparable accuracy.
Insurance coverage varies. Many plans cover DEXA for bone density screening when medically indicated, typically for women over 65 or those with risk factors. Body composition analysis is often not covered. At PrimaryMD, DEXA scans are included in your membership.
DEXA scans require no special preparation. The procedure takes about 15 minutes, involves no injections, and uses very low radiation exposure. Wear comfortable clothing without metal zippers or buttons, and avoid taking calcium supplements the day of your scan.